The FIRST AID modules provide information on caring for injuries and sickness in a backcountry environment when you are hours or even days away from definitive medical care, with focus on what is commonly encountered in the mountains. These modules only provide an overview, but are not meant as adequate instruction for beginners. While traveling in remote, wilderness areas ensure you group includes qualified wilderness medicine professionals, or get a WFA, WAFA or WFR certification yourself.
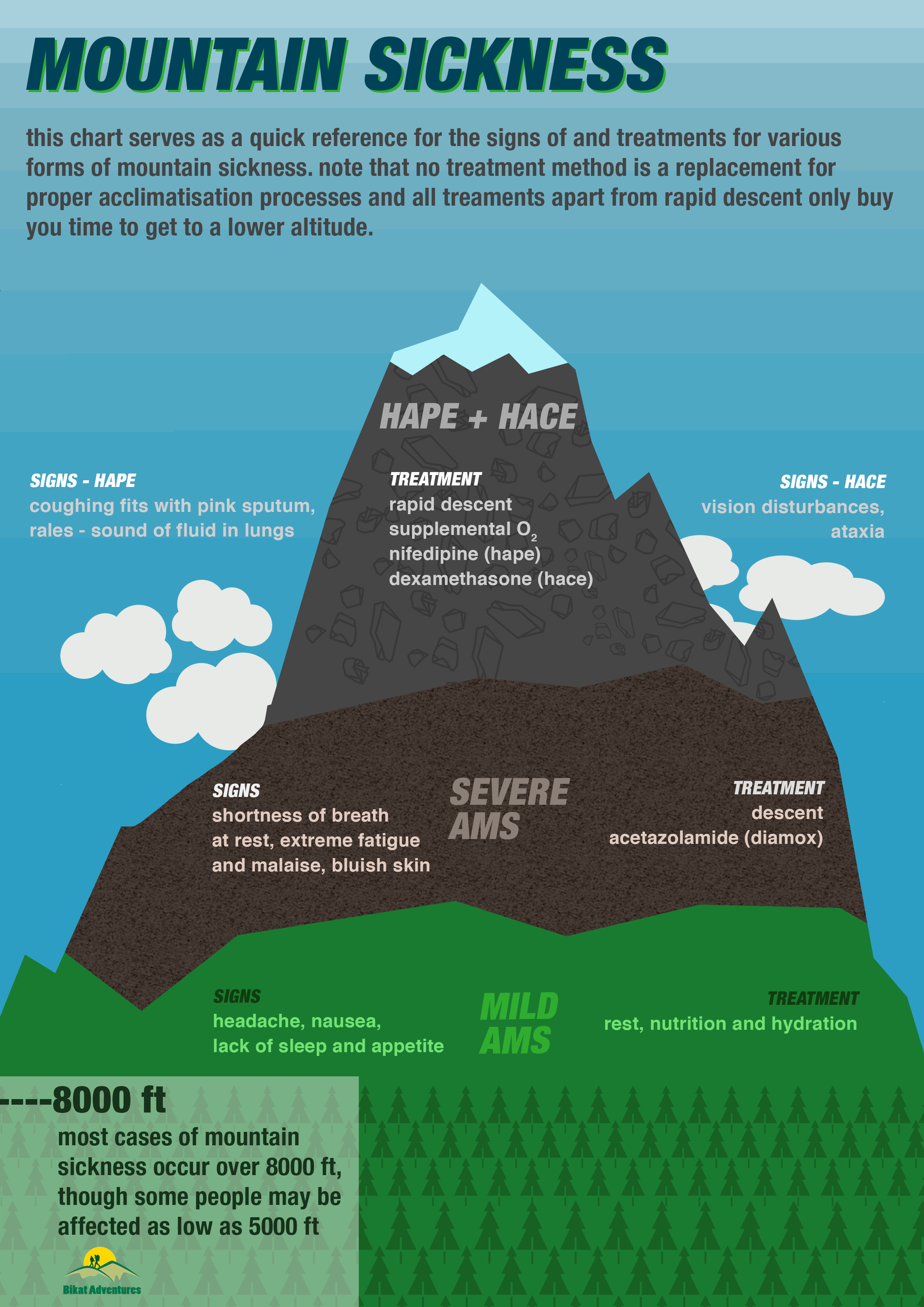
Mountain sickness is a common name for a group of illnesses seen at high elevation due to decreasing oxygen levels and atmospheric pressure. Also called altitude sickness, these affect all people, but to a varying and unpredictable degree.
As oxygen levels decrease, the body compensates rapidly by increasing its respiration rate and depth. This increases blood pH, and in order to maintain the pH balance, the body increases urination. Increased urination, in turn, causes dehydration in a body that is already challenged to maintain hydration. The body gradually acclimatises over a few days to these changes by increasing red blood cell production and oxygen circulation. Severe altitude illnesses occur when the body is not given enough time between rapid altitude gains.
Most cases of mountain sickness are seen at elevations above 10,000 ft, though observed as low as 5,000 ft also.
PREVENTION
- Maintain hydration, despite lack of thirst. Urine colour is a good indicator of hydration. If your urine is darker than clear or pale yellow, it means you are already dehydrated.
- Maintain nutrition despite lack of appetite. As the body faces higher oxygen demands, metabolism - which is not as essential and breathing and circulation - slows down, which decreases appetite. However, more energy is spent during physical exertion at high altitudes, which requires us to replenish energy stores frequently.
- Ascend gradually - the recommended is 2000 ft per day over 8000 ft.
- Camp high, sleep low - do not sleep at the highest altitude you reach in a day. If restriction of camping options forces you to do so, go for acclimatisation walks above your campsite. Do not increase your sleeping altitude by more than 1500 ft per day.
- Pay attention to past history of altitude illness and how your body acclimatizes.
PROPHYLACTIC USE OF DIAMOX
Diamox, or acetazolamide, is a drug commonly prescribed by trekking operators and taken by trekkers or mountaineers going to high altitude. Although how exactly it works is still unknown, it essentially causes hyperventilation - increased frequency and depth of breathing - which is the cornerstone of acclimatisation. There is enough medical research at altitudes upto 6000m to support that prophylactic use of Diamox kick-starts the acclimatisation process.
On the other hand, acetazolamide is also a diuretic (diuretics cause increased urination), the consumption of which requires increased fluid intake of at least 5-6L/day. Often, people are unable to keep up with hydration requirements while consuming diamox, which causes dehydration, and further increases the risk of contracting altitude illness. It is also important to note that use of diamox does not preclude the possibility of altitude illness, nor will it prevent the worsening of altitude illness once it has occured. Side effects of diamox, apart from dehydration, may include tingling in the extremeties, nausea, rashes, and drowsiness.
We recommend against casual prophylactic use of diamox, unless you are flying to from sea level to high altitudes like Leh (in which case acclimatisation is not possible), because of the increased hydration demands it places in an environment where hydration is already a challenge. In addition, it is a prescription drug, and if you do choose to take it, consult your doctor and get a prescription. Acetazolamide must strictly be avoided by people consuming corticosteroids, diabetes patients, people with decreased renal function at sea level and those with sulphonamide allergies because of the adverse reactions it produces in combination with these conditions and the drugs used to treat them.
ACUTE MOUNTAIN SICKNESS
AMS is the most common illness experienced at high altitudes. It can affect people with varying severity depending upon rate of ascent, highest altitude reached and individual physiological factors. The onset is gradual and easy to confuse with other conditions like dehydration or hyponatremia (low sodium levels).
Signs and Symptoms
1. Mild AMS
- Headache - worse in early morning due to decreased respiration while sleeping
- Dizziness
- Nausea
- Fatigue
- Loss of appetite
- Disturbed sleep
2. Severe AMS
- Ataxia - loss of control and coordination
- Cyanosis - blue skin
- Shortness of breath even at rest
- Lassitude and malaise - physical and mental weariness and discomfort
Severe AMS is life threatening and can lead to other forms of altitude illness
HIGH ALTITUDE CEREBRAL EDEMA (HACE)
HACE is basically the progression of the cerebral symptoms of severe AMS. It leads to inflammation, increased intracranial pressure and accumulation of fluid in the brain.
Signs and Symptoms
- Any associated with AMS
- Altered level of responsiveness
- Severe ataxia
- Nausea and vomiting
- Vision disturbances - tunnel vision, partial blindness, black spots, hallucinations
HIGH ALTITUDE PULMONARY EDEMA (HAPE)
HAPE is a progression of AMS in which fluid accumulates in the alveoli and membranes of the lungs, which results in decreased pulmonary function. Easy to misdiagnose as pneumonia, HAPE is the most common cause of non traumatic death at elevation.
Signs and Symptoms
- Any associated with AMS or HACE
- Shortness of breath even at rest
- General weakness
- Splitting headache
- Rales - sound of fluid in lungs, somewhat similar to gurgling
- Coughing fits, progressively more severe, productive and frothy
- Bloody or pink frothy sputum
- Cyanosis - blue skin
- Altered level of responsiveness
TREATMENT FOR ALTITUDE ILLNESSES
- Hydration, rest and nutrition for mild AMS
- Descent for Severe AMS, HAPE or HACE. This is the only definitive treatment for altitude illness. All other treatments only buy you time for descent. Descend at least 1500-3000 ft or further till symptoms subside.
- Supplemental oxygen
- Pressure breathing - pursed lips during exhalation
- Gamow bag - hyperbaric oxygen chambers that simulate altitude descent of upto 5000 ft
- Prescription medicines - acetazolamide (AMS), dexamethasone (HACE), nifedipine (HAPE)
- No single treatment replaces the need for acclimatisation before symptoms appear, or immediate descent once afflicted.
- Descent should be followed by evacuation for all signs and symptoms of severe AMS, HAPE or HACE